Salivary Gland Surgery
There are three named salivary glands in the neck – the parotid, submandibular and sublingual glands. These glands produce saliva at rest and during eating and secrete this saliva into ducts which open into the mouth. The most common glands to need surgical removal are the parotid and submandibular glands.
Salivary duct stones
Sometimes a stone can form in a salivary duct or gland. When this occurs, obstruction to saliva flow can occur with resultant pain and swelling in the affected gland. Sometimes the stone will pass spontaneously and need no treatment. Alternatively, the stone may lodge in the salivary duct and incision into the duct within the mouth is required to extract the stone. If the stone is located within the gland itself necessitating complete removal of the involved gland.
Above: Stone in the right submandibular duct and the typical appearance of an extracted salivary stone
Submandibular gland excision
The submandibular gland sits under the jawbone surrounded by muscles, nerves and blood vessels. There are two main reasons that this gland may need to be removed. Firstly, repetitive inflammation (termed ‘sialadenitis) caused by an impacted stone within the body of the gland or recurrent inflammatory process can lead to frequent pain and swelling. Gland removal may be the best treatment option to manage this condition. Secondly benign and cancerous growths can occur in the submandibular gland and removal of the gland (with or without surrounding lymph nodes) is generally the primary treatment strategy for such pathologies. The submandibular gland is removed through a small incision approximately below your jaw. After submandibular gland surgery, you may be able to go home the same day although A/Prof Sinclair will discuss treatment specifics with you in detail prior to any surgery to ensure you understand the risks, benefits and recovery process of your chosen procedure.
Parotid gland excision
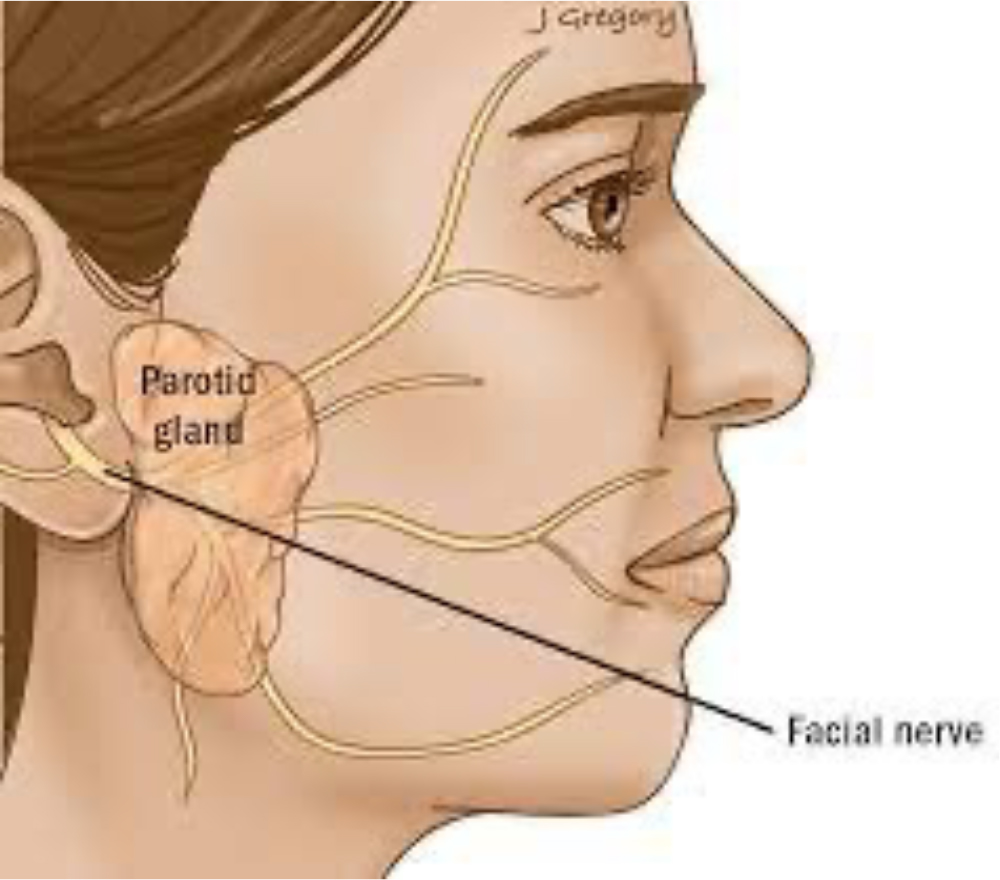
The most common benign (non-cancerous) parotid tumour is called a pleomorphic adenoma. These occur more frequently in women and have the potential to become cancerous if left alone for decades. Warthin’s tumours are the second most common tumour of the parotid gland. These are more common in men and have no ability to become cancerous. Surgery on the parotid gland must be done meticulously due to the close relationship between the parotid gland and facial nerve. The facial nerve is responsible for facial movements and runs through the parotid gland at the junction of its superficial and deep lobes.
The most important step in parotid surgery is careful facial nerve identification and dissection away from the piece of gland to be removed. A/Prof Sinclair is a very experience parotid surgeon and utilizes intraoperative neuromonitoring to map and monitor all facial nerve branches throughout any parotid surgery. This is an added safeguard to ensure that your facial movements after surgery are no different from pre-operatively.
The incision used for parotid surgery extends along the front of the ear and behind the ear into the hairline (see above diagram). Occasionally it will extend into a neck skin crease. This incision heals extremely well and, after 3-6 months, is virtually invisible. A/Prof Sinclair will discuss the cosmesis of the procedure with you in detail before your surgery, including postoperative wound care expectations.
After parotid surgery, you should expect to have some numbness of the skin over the ear lobe and/or angle of the jaw. This occurs because a sensory nerve branch gets cut during the skin incision. Occasionally, you may develop a collection of saliva under the skin due to the cut surfaces of the gland continuing to secrete saliva into the cavity made by the surgery. If this occurs, the saliva can be removed in the office and botulinum toxin injected into the residual gland to prevent further leakage. Afer the surgery, you may also develop sweating during eating on the skin over the parotid gland. This ‘gustatory sweating’ or ‘Frey’s syndrome’, is extremely rare and generally requires no treatment. Other possible risks will be discussed before you sign the procedural consent.